Outbreaks, Symptoms, and Everything Else You Need to Know About the Nipah Virus in Kerala
The first Nipah outbreak occurred in Malaysia and Singapore in 1999. The virus was named after the town in Malaysia where the first epidemic occurred. The Nipah virus is related to the Hendra virus and belongs to the Paramyxoviridae family.
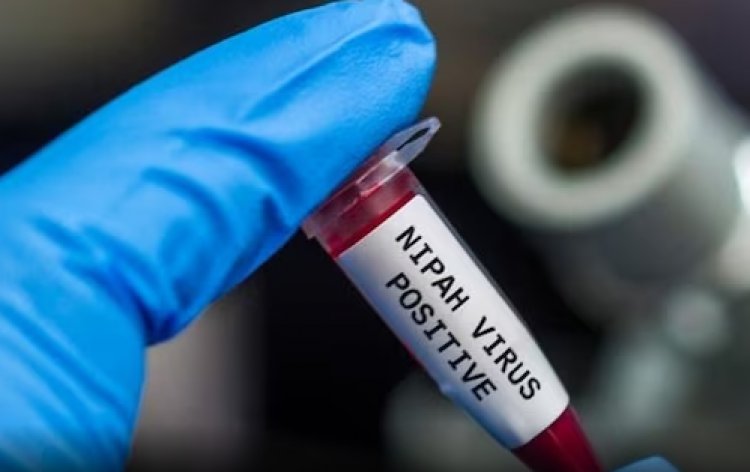
On Tuesday, two deaths were recorded in Kerala's Kozhikode district, reigniting nipah fears in the state. The Union Minister of Health, Mansukh Mandaviya, stated that the Nipah virus was to blame for the deaths.
According to him, four suspected cases are now being followed, and samples from them have been sent to the National Institute of Virology in Pune. As the Nipah scare returns to the state, this page reviews previous Nipah Virus (NiV) outbreaks in India, including symptoms, mechanisms of transmission, and potential prevention measures.
Nipah Virus Outbreaks
The viral infection has previously been discovered five times in India. The National Centres for Disease Control and Prevention classifies Nipah as a zoonotic virus, which means it first spreads between humans and animals.
Nipah's primary animal host reservoir is the fruit bat, commonly known as the flying fox. Fruit bats infected with the virus can transmit it to people and other animals, including pigs. Humans can become infected when they come into contact with ill animals or their body fluids, such as saliva and urine. A'spillover incident' occurs when this happens.
In past outbreaks:
- Siliguri, West Bengal, 2001.
- Nadia, West Bengal, 2007 (100% fatality).
- Kozhikode, Kerala, 2018 (17 deaths).
- Kochi, 2019 (student recovered).
- Pazhur, Kozhikode, 2021 (1 death).
- Recent cases in Kozhikode, Kerala, confirmed as Nipah (2 deaths)
How is the Nipah Virus Spread?
The Nipah virus (NiV) can be transmitted to individuals by:
- Direct contact with diseased animals, like pigs or bats, or their bodily fluids (such blood, urine, or saliva),
- Consuming food items that have been tainted with an infected animal’s bodily fluids (such as fruit tainted with an infected bat’s juice or palm sap).
- Close contact with a NiV-positive individual or their bodily fluids (such as blood, urine, or droplets from the nose or mouth)
Signs and Symptoms
Infection with the Nipah virus (NiV) can cause mild to severe disease, including brain swelling (encephalitis) and even death.
Symptoms often appear 4-14 days following a viral encounter. The sickness commonly begins with 3-14 days of fever and headache and involves signs of a respiratory illness such as coughing, sore throat, and trouble breathing. Drowsiness, disorientation, and mental confusion are frequent symptoms of the subsequent stage of brain swelling (encephalitis), which can rapidly progress to coma within 24-48 hours.
Initial symptoms could involve one or more of the following:
- Fever
- Headache
- Cough
- Sore throat
- Difficulty breathing
- Vomiting
Severe symptoms may occur, including:
- Disorientation, drowsiness, or confusion
- Seizures
- Coma
- Brain swelling (encephalitis)
Death may occur in 40-75% of cases. Long-term unfavourable consequences of Nipah virus infection include persistent convulsions and behavioural problems. Dormant or latent infections, which exhibit symptoms and can end in mortality months or even years after exposure, have also been described.
How Can You Avoid Nipah Virus Infection?
There is currently no recognised therapy or cure for Nipah Virus. As a result, healthcare experts and doctors advise taking necessary steps to avoid Nipah Virus transmission. Several precautions may be taken to limit the danger of Nipah Virus transmission:
- Practice frequent handwashing to prevent germ-related infections.
- Avoid any physical contact with sick animals in your vicinity.
- Steer clear of trees or bushes that serve as natural habitats for bats.
- Refrain from consuming anything that might be contaminated.
- Do not consume fruits that exhibit signs of bat bites.
- Take measures to avoid contact with the saliva, blood, or any other bodily fluids of an infected individual.