Zakir Hussain’s Death from Idiopathic Pulmonary Fibrosis (IPF): Causes, Risks, and Vulnerable Groups
Zakir Hussain’s Death: Tabla maestro Zakir Hussain passed away from idiopathic pulmonary fibrosis, a chronic lung disease characterized by tissue scarring, causing irreversible lung function loss.
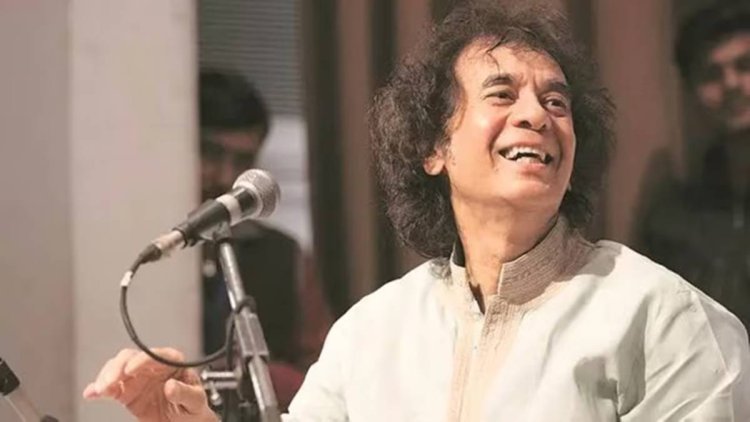
Given that five-time Grammy Award winner and tabla maestro Zakir Hussain died of idiopathic pulmonary fibrosis (IPF) in San Francisco on Sunday, questions have been raised about how this condition occurs and which age group is most susceptible.
It is a chronic, progressive lung disease that causes irreversible loss of lung function due to lung tissue scarring, or fibrosis, according to Dr. Deepak Bhasin is the Senior Director of Critical Care and Pulmonology at Max Hospital in Mohali. Since its precise cause is unknown, IPF is referred to as idiopathic. Because of this scarring, the lungs become thicker and more rigid, which limits their capacity to expand and absorb oxygen.
IPF primarily affects the interstitium, the tissue that surrounds the air sacs (alveoli), which makes it more difficult for oxygen to enter the bloodstream than other lung diseases. Dr. Mahavir Modi, a pulmonologist and sleep specialist at the Ruby Hall Clinic in Pune, adds that this eventually results in chronic dyspnoea, exhaustion, and a lower quality of life.
Why does scarring happen in IPF?
The initial damage to lung tissue is referred to as "idiopathic" (meaning without a clear origin) because the precise cause is unknown. However, scarring is largely a result of the body's healing process. When environmental factors like dust, smoke, or infections, or even autoimmune reactions, cause damage to the lungs, the body tries to heal the damaged tissue.
This repair is controlled and transient in a healthy response. But in IPF, the body overproduces collagen and other fibrous materials, and this repair process becomes dysregulated. According to Dr. Modi, excessive scar tissue develops in place of normal lung tissue regeneration, gradually impairing lung function. IPF is characterised by irreversible scarring as a result of this aberrant healing response.
What are the symptoms?
Breathing becomes difficult due to the stiffening of the lungs caused by fibrosis. Dyspnoea, a dry cough, exhaustion, and weight loss are among the symptoms. Blood oxygen levels gradually decline, leading to complications like heart failure, respiratory failure, or pulmonary hypertension, according to Dr. Bhasin.
Who is at risk?
The majority of cases affect people over 50. IPF affects men a little more frequently than it does women. In certain situations, there may be a genetic component. Smokers, whether present or past, are at higher risk. The risk may rise with prolonged exposure to dust, wood, or metal particles, says Dr. Bhasin. "People with chronic GERD who repeatedly microaspirate stomach acid may eventually develop lung tissue damage," Dr. Modi continues.
How is IPF diagnosed?
The diagnosis can occasionally be confirmed by lung biopsy, pulmonary function tests, and high-resolution CT scans. "However, it is crucial to rule out other causes of lung diseases," Dr. Bhasin says.
How is the condition managed?
Dr. Bhasin says antifibrotic medications like nintedanib and pirfenidone slow the progression of the disease. Lung exercises and oxygen therapy are added to this. According to him, "in more advanced cases, lung transplantation may be considered." For this reason, Dr. Modi says,Early diagnosis and multidisciplinary care are critical.”